Nowadays, countless people around the world suffer from insomnia - a sleep disorder that is often underestimated. The underlying mechanisms of insomnia are complex, and its causes are diverse. In recent years, an increasing number of studies have begun exploring the potential of the Quality 1.5 ata hyperbaric chamber for sale in promoting better sleep. This article will analyze the feasibility of improving insomnia symptoms through the hyperbaric oxygen chamber 1.5 ATA from three key perspectives: mechanism, target population, and treatment considerations.
Mechanism: How Does Hyperbaric Oxygen Therapy Improve Sleep?
1. Enhancing Cerebral Oxygen Metabolism and Microcirculation
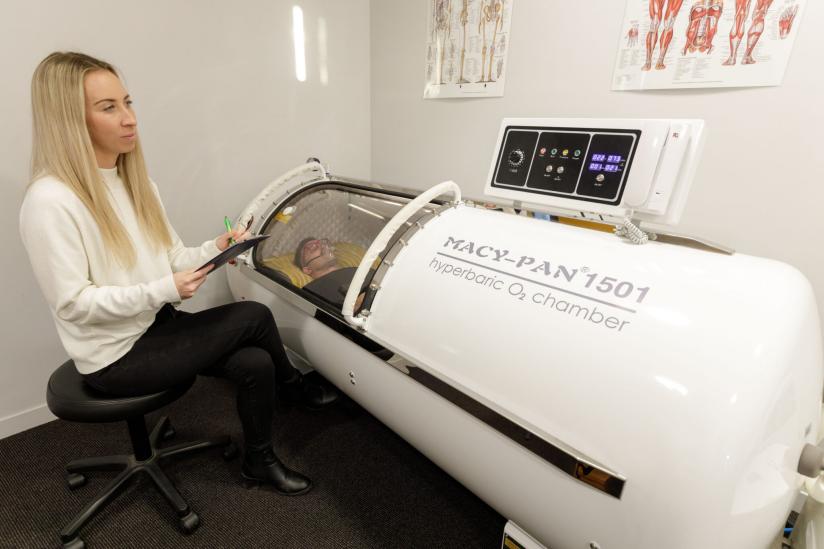
The principle of hyperbaric oxygen therapy (HBOT) lies in breathing nearly 100% oxygen under a pressurized environment within the High-Quality hard sided hyperbaric chamber 1.5 ATA . This process significantly increases the partial pressure of oxygen, thereby elevating the amount of dissolved oxygen in the blood. Studies have shown that the increased oxygen intake helps improve cerebral oxygenation and supports neuronal metabolism.
In cases of sleep disorders, reduced cerebral oxygen metabolism and insufficient microvascular perfusion may be overlooked contributing factors. Theoretically, enhancing tissue oxygenation can promote neural repair and alleviate inflammatory responses, thereby increasing the duration of deep sleep (slow-wave sleep).
2. Regulating Neurotransmitters and Repairing Neural Damage
Clinical studies have shown that hyperbaric oxygen therapy (HBOT) can serve as an adjunctive treatment to improve sleep quality in certain sleep disorders caused by brain injury, cerebrovascular events, or neurodegenerative diseases. For example, among patients with Parkinson’s disease, HBOT combined with conventional therapy has been found to improve indicators such as the Pittsburgh Sleep Quality Index (PSQI).
In addition, ongoing systematic reviews on post-stroke patients with insomnia suggest that HBOT may act on the neurotrophic-inflammation-oxidative stress axis, thereby helping to improve sleep quality.
3. Reducing Inflammation and Promoting Metabolic Waste Clearance
The brain’s glymphatic system is responsible for clearing metabolic waste and becomes particularly active during sleep. Some studies suggest that HBOT may enhance this process by improving cerebral perfusion and boosting mitochondrial activity, thereby supporting restorative sleep.
In summary, the above mechanisms indicate that hyperbaric oxygen therapy may theoretically serve as an effective tool for improving certain types of insomnia. However, it is important to emphasize that current research positions HBOT primarily as an adjunctive or supplementary therapy, rather than a first-line or universally applicable treatment for insomnia.
Which Groups Are More Suitable for Considering Hyperbaric Oxygen Therapy for Insomnia?

Clinical studies have found that not all individuals with insomnia are suitable candidates for hyperbaric oxygen therapy (HBOT). The following groups may be more appropriate, though careful evaluation is still required:
1. Individuals with Neurological Disorders:
Those experiencing sleep disturbances secondary to conditions such as traumatic brain injury (TBI), mild traumatic brain injury (mTBI), post-stroke sequelae, or Parkinson’s disease. Research indicates that these individuals often exhibit impaired cerebral oxygen metabolism or neurotrophic dysfunction, for which HBOT may serve as a supportive treatment.
2. Individuals with Insomnia in Chronic High-Altitude or Hypoxic Conditions:
A randomized trial reported that a 10-day course of HBOT significantly improved both PSQI (Pittsburgh Sleep Quality Index) and ISI (Insomnia Severity Index) scores among chronic insomnia patients living in high-altitude regions.
3. Individuals with Chronic Fatigue, Recovery Needs, or Reduced Oxygenation:
This includes people experiencing long-term fatigue, chronic pain, post-surgical recovery, or neuroendocrine imbalance. Some wellness centers also classify such individuals as potentially suitable candidates for HBOT.
At the same time, it is important to clarify which individuals should use HBOT with caution and which require case-by-case evaluation:
1. Use with Caution:
Individuals with acute otitis media, eardrum issues, severe pulmonary disease, inability to tolerate pressurized environments, or uncontrolled severe epilepsy may face a risk of central nervous system oxygen toxicity if they undergo hyperbaric oxygen therapy.
2. Case-by-Case Evaluation:
Individuals whose insomnia is purely psychological or behavioral (e.g., primary insomnia) and can be improved simply by proper bed rest, without any organic cause, should first receive standard Cognitive Behavioral Therapy for Insomnia (CBT-I) before considering HBOT.
Treatment Protocol Design and Considerations

1. Treatment Frequency and Duration
According to current literature, for specific populations, HBOT for sleep improvement is typically administered once daily or every other day for 4-6 weeks. For example, in studies on high-altitude insomnia, a 10-day course was used.
Professional hyperbaric oxygen therapy providers often design a “base course + maintenance course” model: sessions last 60-90 minutes, 3-5 times per week for 4-6 weeks, with frequency adjustments made based on individual sleep improvement.
2. Safety and Contraindications
l Prior to treatment, assess hearing, sinuses, pulmonary and cardiac function, and history of epilepsy.
l During treatment, monitor for ear and sinus discomfort due to pressure changes, and perform tympanic membrane ventilation as needed.
l Avoid bringing flammable items, cosmetics, perfumes, or battery-powered devices into a sealed high-oxygen environment.
l Long-term or high-frequency sessions may increase the risk of oxygen toxicity, visual changes, or pulmonary barotrauma. Although rare, these risks require physician supervision.
3. Efficacy Monitoring and Adjustment
l Establish baseline sleep quality indicators, such as PSQI, ISI, nighttime awakenings, and subjective sleep quality.
l Reassess these indicators every 1–2 weeks during treatment. If improvement is minimal, evaluate for coexisting sleep disorders (e.g., OSA, genetic insomnia, psychological factors) and adjust the treatment plan accordingly.
l If adverse effects occur (e.g., ear pain, dizziness, blurred vision), pause treatment and have a physician evaluate.
4. Combined Lifestyle Interventions
HBOT is not an “isolated therapy.” The lifestyle habits of individuals with insomnia or other HBOT recipients can influence treatment efficacy. Therefore, patients should maintain good sleep hygiene, follow a regular daily routine, and limit intake of stimulants such as caffeine or alcohol at night to help manage anxiety and stress.
Only by combining mechanistic therapy with behavioral interventions can sleep quality be truly improved.
Here’s a polished English translation of your text:
Conclusion
In summary, hyperbaric oxygen therapy (HBOT) has potential for improving insomnia in individuals with underlying brain injury, hypoxic conditions, or neurotrophic deficits. Its mechanism is scientifically plausible, and preliminary research supports its role as an adjunctive treatment. However, HBOT is not a “universal remedy” for insomnia, and it is important to note that:
l Hyperbaric oxygen therapy (HBOT) is not currently considered a first-line or routinely recommended treatment for most cases of insomnia that are primarily psychological or behavioral in nature.
l Although treatment frequency and course duration have been discussed previously, there is still no standardized consensus regarding the magnitude of efficacy, duration of effect, or optimal treatment frequency.
l Many hospitals, private clinics, and wellness centers are equipped with macy pan hbot, which insomnia patients can experience. Home-use hyperbaric chambers are also available, but their cost, safety, accessibility, and suitability for individual patients should be evaluated by a qualified physician on a case-by-case basis.


Post time: Oct-22-2025

